There are few things more humbling than sitting in an oncologist’s office, waiting to be told if your life-saving drugs are working.
It’s even more vulnerable-making when a massive red herring is thrown into the mix right before your appointment.
When I go to the hospital every fourth Tuesday, I have blood tests, followed by weight and blood pressure observations, then an ECG to check on my heart before my next course of Ribociclib, then the consultation, then my monthly Zoladex implant. Great.
Only this time, someone came out and told me I didn’t need the ECG. I took this to be a Very Bad Sign, eg I didn’t need the ECG because the Ribociclib wasn’t working and I wouldn’t be continuing it.
(My reasoning was rather like in June, when I’d been told the suspicious lesion in my sternum was probably not of concern, then I received a text message with my first oncology consultation in years and immediately knew the cancer was back.)
I had been very positive up to that point, but I was now very much on edge.
There is always a long, long wait between bloods and consultation. It’s meant to be 90 minutes to get the blood results back, but it’s usually closer to three hours, during which time your bladder fills up but you don’t want to pop to the loo lest you miss your appointment, then you spend the actual appointment trying not to wet yourself.
I don’t begrudge the NHS at all – they are massively overstretched – but when you’re waiting for particularly important results eg the literal difference between life and death, it is agonising.
I comforted myself with the theory that if it was bad news, they wouldn’t make us wait, and as we went an hour beyond my appointment time, I became marginally less anxious. That quickly ended, though, when the lady next to us decided it was appropriate to start watching something called Murder Detectives out loud on her phone. I managed one chapter of my book before giving up.
We were then led into a different room from the one where we normally have the consultations. In that heightened state, you need your normal routines to keep you feeling safe, and this threw me further off-kilter. I knew it was probably just that another patient was in our normal room, but still, every little change can leave you further on edge.
By this point, I was on the verge of tears, and Mark and I could barely process another thought until we heard whatever news they were about to deliver.
Then in walked the young doctor, and within seconds I heard the following words:
— ‘There’s been an almost complete metabolic response.’
Now, this sounded like a positive, but my head was all over the place. So I asked him, over the next 20 minutes, in all the different ways I could think of:
— ‘Does that mean the tumour has almost gone?’
— ‘So the drugs are working?’
— ‘Sorry, did you say the cancer in my sternum has almost disappeared?’
— ‘And you didn’t find any cancer anywhere else in the body?’ (At this point, I’ve clearly taken on hospital parlance and started referring to my body as ‘the body’.)
He said some of the following things, and I paraphrase because I was delirious:
— ‘The area where the tumour was has almost completely resolved.’
— ‘It’s as good a result as you could possibly expect.’
— ‘There is no cancer anywhere else in the body.’
Then he said some Very, Very Hopeful Things that I am afraid to even repeat for fear of jinxing it.
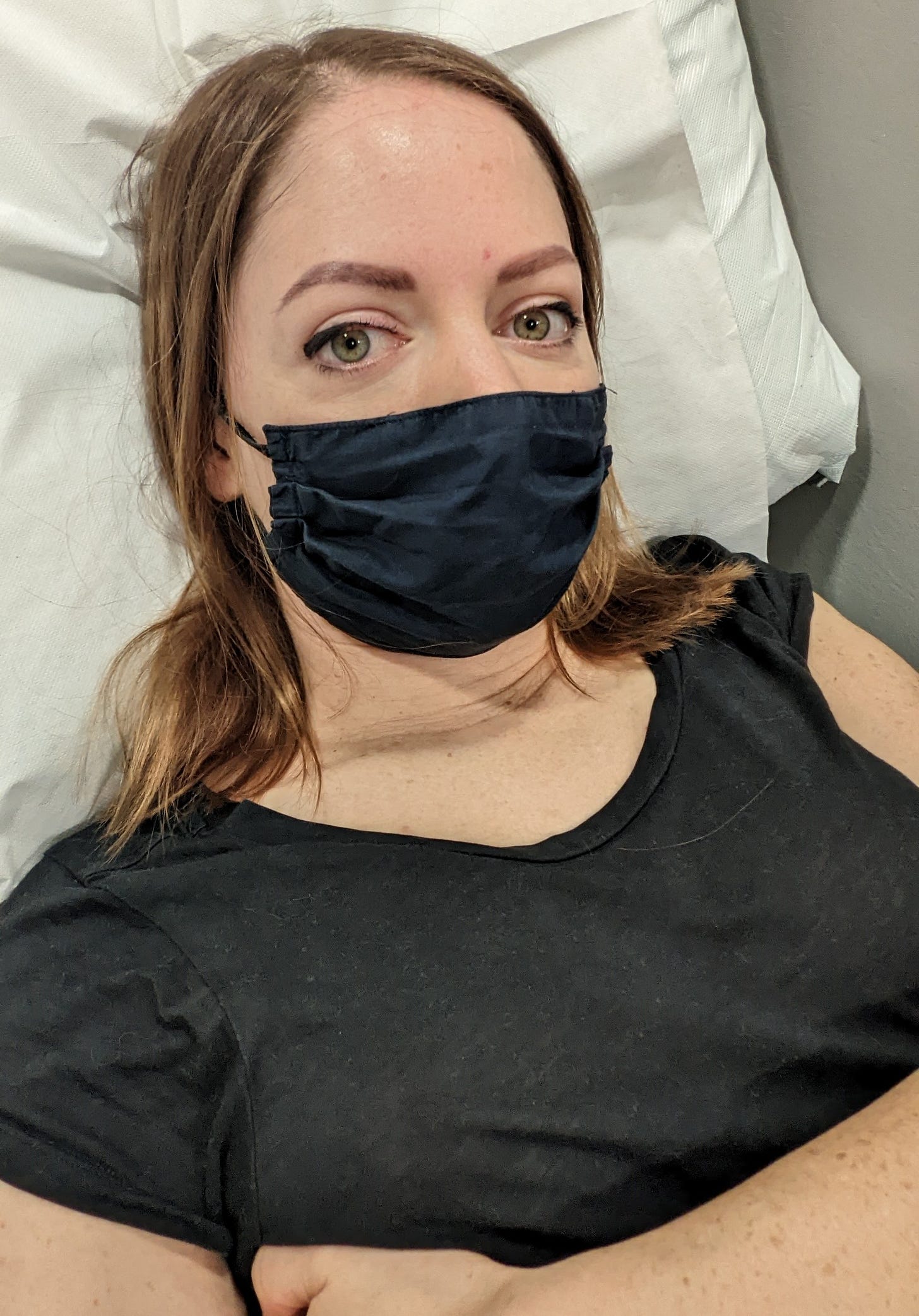
This was my face:
I mean, I was expecting good news. I was in a lot of pain between October 2021 and August 2022, and that pain has reduced so dramatically that the drugs must be working. In Portugal in August, I remember sneezing and feeling like I’d been hit in the chest with a sledgehammer; I now sneeze pain-free.
But they had told me that occasionally, after several months on the drugs, the PET-CT scan can reveal scars elsewhere in the body, indicating that the cancer may be more widespread than first thought.
Also, although I don’t have the same pain in my sternum, I have a dull feeling that goes right across my chest, and there was a niggling feeling that it could be cancer. (I now think it is probably just the scars healing.)
Next steps and second chances
It may sound dramatic, but I feel like I’ve been given a second chance. Over the last few months, I’ve had so many horrible thoughts about my potentially very-much-shortened life, and I feel like I’ve been granted more time. Over the last few days, I’ve made good progress with my second novel, and I am so excited to think that I’ll be around to finish it and hopefully see it published (and more books after that).
I still have incurable, stage four breast cancer, and the cancer will still come back eventually. I still have to have scans every three months for the rest of my life.
BUT the fact that my body has responded so positively to this first course of treatment really gives me so much hope for the future.
On the way to our results appointment on Tuesday, Mark and I visited one of several wedding venues. It was POURING with rain – a truly grim, grim day – and I had already said that if the news was bad, there was no way we’d be getting married there. But the venue was stunning and I now feel like I can throw some of my energy into planning the wedding (and honeymoon!) that we very much deserve.
The next step is thoracic surgery. This isn’t yet confirmed, but the idea is that by removing a large area where the tumour was, we have a greater chance of keeping the cancer away for much longer than if I continued on the drugs alone.
It’s a big surgery with a long recovery period, so I am pretty nervous, but ultimately it’s great news that I’m even being considered for it, because if the cancer hadn’t shrunk, or if it had spread to other parts of my body, it’s unlikely I’d have been able to have surgery at all.
Scanxiety
Returning to the PET-CT scan waiting room last Thursday brought back the trauma I felt when I went there in June after 10 years cancer-free. It was just a few days after my 10th anniversary and I’d been told the lesion that had been detected in my MRI scan might be some sort of post-radiotherapy bone thing (I think the word ‘necrosis’ was mentioned, which sounded awful, but marginally nicer than stage four cancer).
In hindsight, I am certain they knew it was cancer and that that was just an attempt to put my mind at ease. (You know it’s pretty bad when the word ‘necrosis’ is considered mind-easing.)
In that waiting room in June, the other two patients were discussing their metastatic (stage four) cancers, and I was the one eavesdropping while desperately hoping I didn’t have cancer too. Going back this time as a metastatic cancer patient made me feel naive for even considering it might not be cancer, but of course the mind goes to all sorts of places to protect one’s sanity.
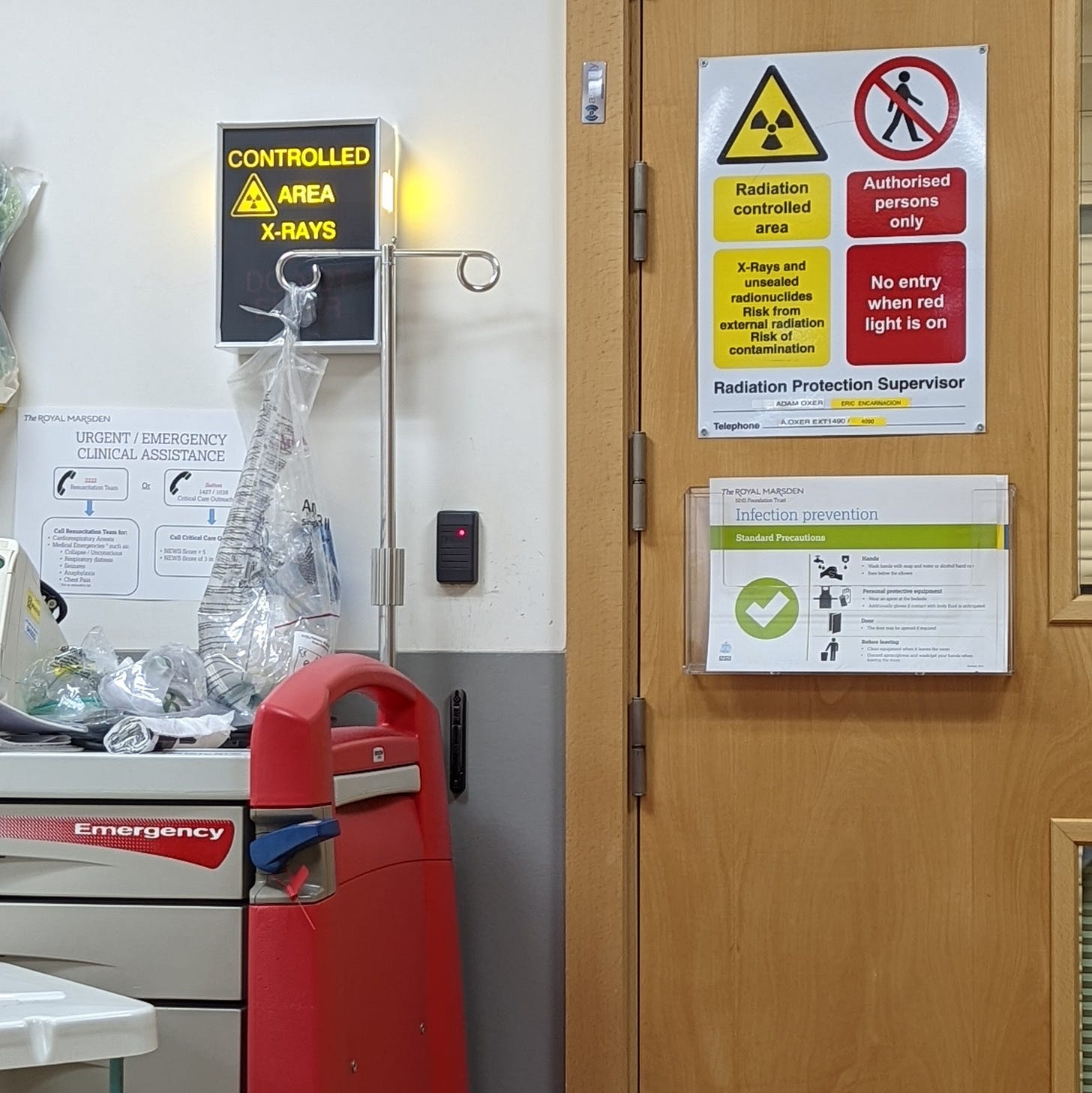
Below is the syringe they use to inject you with radioactive glucose dye, which allows the cancer cells to show up on the PET-CT scan imagery. (They present it to you in a big steel box, I think to protect everyone from the radiation.)
You have to fast for six hours beforehand to starve your cells of food. Because they are fast-growing, cancer cells are extra hungry, so they gobble up the glucose before it can get to the rest of your cells, meaning the cancer glows brightly on the scan.
You then lie horizontal for an hour while the substance works its way around your body. I was able to read my book, but people have since told me their hospitals make them lie completely still in a dark room, as even reading a book can stimulate your brain cells and cause the glucose to go straight to your brain, or something like that.
For the scan itself, you lie still for about 20 minutes and just wait. It’s very quiet, compared with an MRI scan, which is like lying down in the middle of a building site. It is painless – the only slight discomfort is having a cannula fitted, but if they do it right, you barely feel it.
For 24 hours after the scan, you’re not allowed to go near pregnant women or young children because of the radioactive substance inside you. I asked why it wasn’t dangerous to cats, and was told it’s because they don’t live long enough to feel the effects, which is sad, because I wish cats could live forever.
We only had to wait four days for the scan result, and we had plans to go away for Mark’s birthday to a fancy restaurant with rooms called Jöro in Sheffield. It was suitably wonderful, and we got completely soaked in the rain at the top of Mam Tor in the Peak District on Sunday. It was just what we needed.
I am elated about these results, but I’m also realistic and cautious about the future. It’s a huge milestone knowing that my first scan was a good scan – we both (and my mum and dad) needed this fuel to get through everything else that’s to come.
There will be many, many more mountains to climb, but we’ll do it together, step by step (and Mark will probably be wearing shorts and inappropriate footwear).
A quick word on secondary breast cancer:
I am beyond grateful to my oncologist and the whole team at the Royal Marsden, and to the scientists who created drugs like Zoladex, Letrozole and Ribociclib. But there are thought to be 35,000 people living with secondary breast cancer in the UK alone, and unfortunately the time and money invested in treatments and cures is nothing like what goes into primary care treatment. We need more funding, more research and more attention. There’s more about this on Breast Cancer Now and MetUpUK.







Such wonderful news, so pleased for you!
Such good news!
You know how to build suspense too..